
Most of these won’t benefit most of the people who take them.
I recently wrote an article about statin denialism for Skeptical Inquirer. I showed that there is compelling evidence that statins reduce the incidence of heart attacks when prescribed for patients with existing disease or at high risk. I addressed some of the ridiculous claims from denialists who reject the evidence and demonize statins. They say the evidence was 100% fabricated, and statins are worthless. They claim that nearly half of patients experience devastating side effects (but strangely these don’t show up in controlled studies!). They even resort to nonsense like the claim that table salt is 1/3 glass and 1/3 sand, and the glass particles are cutting the linings of our arteries and making them bleed!
I received an inquiry from a reader who was prescribed statins appropriately, for existing cardiovascular disease, but was one of the few unlucky patients who have to stop the drugs because of intolerable side effects. He sent me an article from New Scientist that made him question the effectiveness of statins and the incidence of side effects. It was not a scientific study, but a “cover story” by Michael Brooks, a journalist with a PhD in quantum physics. The article is built around his personal experience; he stopped taking statins because of muscle pain but is planning to try a different statin. He is not anti-statin. He concludes, “But I certainly won’t see them as the cure-all I once did.” That’s something of a straw man; no one should ever have seen them as a cure-all.
The part that shocked my correspondent was that Brooks’ claim that 96% of patients with existing heart disease and 98% of those without heart disease got no benefit from statins. Why would anyone want to take a drug that is so unlikely to help them? In the first place, those numbers are misleading (see below); and in the second place, most patients get no benefit from most drugs. That’s an important and often-misunderstood fact; I’ll get back to it shortly, but first let’s take a closer look at the New Scientist article.
The “Cholesterol Wars” article
The author says he was “vaguely aware” of a backlash against statins and against the role of cholesterol in heart disease. He set out to do his own investigation. It is difficult for someone with no background in the field to master all the data and the issues involved, and I think he was misled by some of what he found in his research. He cites the 1913 Russian experiment where rabbits were fed a high-cholesterol diet and developed atherosclerosis; but he doesn’t point out that animal research is problematic and doesn’t always translate to human conclusions. In fact, over a century later, no research has found that humans respond to a high cholesterol diet in the same way as those Russian rabbits.
His analysis is fairly well balanced overall. He points out that many factors beyond blood cholesterol determine how healthy your heart is. That’s common knowledge, and the statin treatment guidelines emphasize the importance of lifestyle factors like exercise, smoking cessation, and weight control. These should be tried before resorting to statins and should be continued during statin treatment.
He quotes Uffe Ravnskov, notorious cholesterol skeptic, who calls the cholesterol campaign “the greatest medical scandal in modern times.” Ravnskov claims there is no link between cholesterol and atherosclerosis. He is demonstrably wrong. To be fair, Brooks also quotes an expert who says those who deny a link are talking complete nonsense.
Brooks accurately reports the evidence showing that statins indisputably save lives for patients with existing heart disease, and to a lesser extent, for those without existing disease who are high-risk. Even if they don’t live longer, they are less likely to have non-fatal heart attacks.
He discusses the differing estimates of muscle pain side effects: a systematic review found that less than one percent were affected, but many estimates are much higher. Real-world patients report a higher incidence of muscle side effects than the patients in clinical trials. This bothers me. I suspect the true incidence is higher than one percent, but unsolicited self-reports from patients on statins are meaningless without a control group for comparison. Better-designed large long-term controlled studies will be needed to pin down the true incidence. At any rate, the incidence of side effects is not high, and even the most serious complication, rhabdomyolysis, can usually be reversed by stopping the drug.
He acknowledges that concerns about statins causing diabetes are less solid, and may be an artefact of the way we define diabetes.
He agrees that patients with existing disease should take statins, but he says it’s far from obvious that the rest of us should. Lumping patients without existing disease into “the rest of us” is misleading. No reputable authority is recommending statins for everyone, or for low risk patients; and the benefits of statins vary widely with the individual patient’s risk factors. Some patients at low risk should not take statins; many patients at high risk should, and the greater the risk, the greater the benefit.
His major problem with statins is that most patients will not benefit, and we can’t predict which ones will, so it’s like a lottery. But that’s true of all medicines.
Most patients don’t benefit from most drugs
Yes, you read that right! Most patients don’t benefit from most drugs. This can be expressed as the NNT, the number needed to treat for one person to benefit. I don’t know where Brooks got his “no benefit for 98% and 96%” statistics, but that would translate to NNTs of 50 and 25, respectively. There is a website where you can look up the NNT for various treatments. According to that website, 60 people without heart disease have to be treated with statins for 5 years to prevent one heart attack. For people who already have heart disease, the NNT to prevent one non-fatal heart attack is 39, and the NNT to save one life is 83, even worse than what Brooks said. But looking at the numbers this way is misleading because it is based on averages. If someone has fewer risk factors than average, the NNT will be larger; and if a patient has many risk factors, the NNT will be smaller.
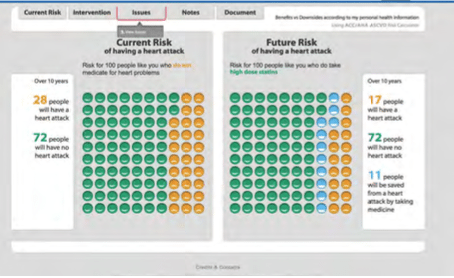
There is a convenient decision aid available online from the Mayo Clinic. In my Skeptical Inquirer article, I showed the following results for a hypothetical patient: a middle-aged man with several risk factors. The left panel shows what can be expected for 100 patients with a similar risk profile: without treatment, 28 will have a heart attack and 72 will not. The right panel shows that with statin treatment, only 17 will have a heart attack, and 11 people will be spared a heart attack because of the treatment. In this case, 100 patients are treated to prevent 11 heart attacks, for an NNT of 9.
Just for kicks, I went back to the decision aid and put in the numbers for a really high-risk hypothetical man, and got an NNT of 4. And I put in the numbers for a hypothetical young woman with no risk factors at all, and it showed that there would be no benefit at all; it would be useless for her to take statins.
Some of these NNTs may seem alarming high to you, but let’s put them into perspective with some other common medical treatments addressed on the NNT website:
- Blood pressure medications for 5 years:
- NNT to prevent one death: 125
- NNT to prevent one stroke: 67
- NNT to prevent one heart attack: 100
- Antibiotics for sinusitis: NNT 18
- Antibiotics to prevent infection with a broken bone that pierces the skin: NNT 16
- Defibrillation for cardiac arrest: NNT 2.5
- Warfarin for 1.5 years in patients with atrial fibrillation: NNT 25 to prevent one stroke, NNT 42 to prevent one death from any cause
- CT lung cancer screening in high-risk smokers: NNT 217 to prevent one death
- Aspirin daily for one year
- For healthy people: NNT to prevent one stroke or heart attack: 1,667
- For people with a prior heart attack: NNT 77 to prevent one heart attack, 200 to prevent one stroke
For many conditions, no benefit was found:
- Antibiotics for acute ear infection
- Antibiotics for acute bronchitis
- Antibiotics for animal bites
- Antivirals to prevent post-herpetic neuralgia
- Epidural steroids for sciatica
- PSA test
- Screening mammogram
- Biphosphonates to prevent fracture in post-menopausal women
You may find some of these hard to accept; but for each, the NNT website provides a detailed, nuanced discussion and shows where the numbers come from.
I tried to think of a treatment that consistently benefited everyone.
- Penicillin for syphilis? Nope; I found a reported treatment failure rate of 22%
- Insulin for type 1 diabetes? I couldn’t find an NNT. These patients will die without insulin, but some patients die even with treatment.
NNT isn’t everything
There are other considerations:
- NNT only reflects binary outcomes; not continuous ones (i.e. survival vs. death from high blood pressure rather than how much BP is lowered).
- Most therapies impact more than one outcome
- The calculations are time-dependent
- Benefits will vary with baseline risk
- The NNH (number needed to harm) must be taken into consideration
- Patients’ values must be considered when deciding whether to treat
- Individual patients seen in a doctor’s office may differ from study populations
- The acceptability of an NNT depends on a lot of factors. “A number needed to treat of 100 may be acceptable for a drug that is cheap, easy to take and has few side effects; however, a number needed to treat of 5 may be too high for an expensive drug that carries substantial potential toxicities.”
Doctors tend not to think about NNT
Most patients do not benefit from most drugs. Doctors know this, but that doesn’t stop them from prescribing. Some patients do benefit from most drugs; after all, pharmaceuticals have to demonstrate benefit before the FDA will approve them for marketing. Doctors tend not to think in terms of NNT. They think in terms of who will benefit, not in terms of who won’t. They have to act without having all the information. There is no way of knowing which patients will benefit, so we are stuck treating the many to benefit the few. Brooks compares it to entering a lottery, but I prefer to compare it to deciding whether to buy insurance. Most of us pay for fire insurance for our homes, but not many houses burn down. We willingly pay premiums that may never benefit us because the cost of an uninsured disaster is so great.
The placebo factor
An argument can be made for de-emphasizing the NNT and letting patients believe the treatment will work for them. Perhaps this is one of the places where doctors could take advantage of the placebo response by giving patients higher expectations. As we have pointed out many times, prescribing inert placebos is unethical; but trying to maximize the contextual effects of the therapeutic encounter for an effective treatment is not.
Conclusion: Not a problem
In short, while the figures presented in Brooks’ article for “no benefit from statins” may sound alarming, they should not be. Most patients do not benefit from most drugs, and the numbers for statins are well within the range of the numbers for many other standard drugs. Perhaps someday genomic analysis or other advances may help us predict which patients will benefit; but until then, we are stuck treating the many to help the few. But that doesn’t mean we should treat indiscriminately or add statins to the drinking water. We know enough to prescribe statins selectively based on risk analyses like the Mayo Clinic decision aids. Still a lottery, but we can improve the odds.
